The cornea is the clear, living tissue on the very front part of the eye. Light passes through the clear cornea on its path toward the retina in the back part of the eye. A healthy, clear cornea is necessary for perfectly clear vision. Sometimes, the cornea is referred to as the “window” to the eye. Occasionally, either through disease or injury, the corneal tissue is damaged to a point where light can no longer effectively pass through it, resulting in reduced vision. Where indicated by an ophthalmologist, a corneal transplant procedure may be performed which replaces the damaged cornea with a clear donor cornea. Typically, patients with corneal diseases were required to have a full thickness corneal transplant, or penetrating keratoplasty (PK), in order to improve their vision.
Some diseases of the cornea, however, only affect the inner lining of the cornea. Therefore, a new version of corneal transplant, known as a Descemet’s Stripping Endothelial Keratoplasty (DSEK), has been introduced as a new surgical method that uses only a very thin portion of the cornea for transplant. DSEK is a corneal transplant technique where the unhealthy, diseased, posterior portion of a patient’s cornea is removed and replaced with healthy donor tissue obtained from the eye bank. Unlike the PK, the DSEK procedure utilizes a much smaller surgical incision and requires no corneal sutures. This usually results in more rapid visual rehabilitation for the patient and also reduces the risk of sight threatening complications that may occur with the PK.
When endothelial cells are healthy, they function as a “pump-leak system” to provide nourishment for the cornea. In other words these cells allow nourishing fluid from inside the eye (aqueous humor) to leak into the cornea. After the corneal cells have been nourished, the cells pump the fluid out of the cornea. If the endothelial pump is compromised for any reason the cornea will over hydrate and become cloudy. This most commonly occurs in patients who have sustained trauma to the endothelial layer during complicated cataract surgery or patients who have an inherited disease of the corneal endothelium known as Fuchs’ Endothelial Dystrophy.
When the corneal endothelium is stressed, the endothelial cells become larger and more sparse. As endothelial cell density falls between 500 to 1000 cells/mm, the pump mechanism can no longer maintain a clear cornea. In the case of Fuchs’ dystrophy the endothelial cells also start secreting material that makes Descemet’s layer thicker and more opaque. Vision eventually deteriorates to a point where these patients feel like they are looking through wax paper. Such patients are good candidates for the DSEK procedure.
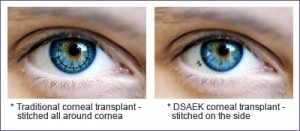
A full thickness corneal transplant removes a circular disc from the center of the cornea. A healthy, clear donor cornea is obtained from a donor cadaver. This donor cornea then has the central circular area removed with a similar shape. The new cornea is then put into position and sutured into place. A full thickness corneal transplant is a safe and well tolerated procedure. However, the recovery can be quite long, up to twelve months. It is also not uncommon to have significant irregular curvature of the cornea because of the sutures. In many cases a contact lens is required to achieve the best vision. Finally, a full thickness transplant can have continued weakness even years later such that a minor trauma can dislocate the graft from its position.
The DSEK procedure can overcome many of these problems associated with a standard corneal transplant. With a DSEK procedure only the abnormal inner lining of the cornea is removed. A thin, circular disc is then removed from the inner lining of a donor cornea. This is folded and place inside of the eye where an air bubble pushes it in place until it heals in an appropriate position. No sutures are required and the structure of the cornea remains intact, leading to a faster visual recovery and less astigmatism.
With either procedure there is a risk of rejection, where the body’s immune system starts to fight against the cornea. The symptoms of rejection are redness, blurry vision, and light sensitivity. This can happen at any time months or years after the transplant. A complication that can occur from the DSEK procedure that is not associated with a standard transplant is a graft dislocation, where the circular disc slips from its intended position. In this circumstance the donor disc needs to be repositioned in the operating room.
The DSEK procedure is done under local anesthesia. The patient is brought to the operating room in an ambulatory surgery center. Relaxing medications are put in the vein and numbing injections placed around the eye. The procedure takes approximately 45 minutes. For the first 24 hours you will be asked to lie on your back with your face pointed directly to the ceiling for as much time as you can tolerate. This will help the graft stay in position as the air bubble holds it up into place on your cornea. You will be given several drops to use to prevent infection as well as to help the eye heal comfortably. After the first 48 hours there are minimal restrictions to your activities. The vision is usually better within one week. 80% of the healing has taken place by one month but the vision can continue to slowly improve over the next four to six month. Dr. Melki is one of the first surgeons in Boston to perform the DSEK procedure and has had amazing results successfully improving the vision of patients with corneal disease.
